Suggest an improvement
var gform;gform||(document.addEventListener(“gform_main_scripts_loaded”,function()gform.scriptsLoaded=!0),document.addEventListener(“gform/theme/scripts_loaded”,function()gform.themeScriptsLoaded=!0),window.addEventListener(“DOMContentLoaded”,function()gform.domLoaded=!0),gform=domLoaded:!1,scriptsLoaded:!1,themeScriptsLoaded:!1,isFormEditor:()=>”function”==typeof InitializeEditor,callIfLoaded:function(o)!gform.themeScriptsLoaded&&!gform.isFormEditor(),initializeOnLoaded:function(o)(document.addEventListener(“gform_main_scripts_loaded”,()=>gform.scriptsLoaded=!0,gform.callIfLoaded(o)),document.addEventListener(“gform/theme/scripts_loaded”,()=>gform.themeScriptsLoaded=!0,gform.callIfLoaded(o)),window.addEventListener(“DOMContentLoaded”,()=>gform.domLoaded=!0,gform.callIfLoaded(o))),hooks:action:,filter:,addAction:function(o,r,e,t)gform.addHook(“action”,o,r,e,t),addFilter:function(o,r,e,t)gform.addHook(“filter”,o,r,e,t),doAction:function(o)gform.doHook(“action”,o,arguments),applyFilters:function(o)return gform.doHook(“filter”,o,arguments),removeAction:function(o,r)gform.removeHook(“action”,o,r),removeFilter:function(o,r,e)gform.removeHook(“filter”,o,r,e),addHook:function(o,r,e,t,n)null==gform.hooks[o][r]&&(gform.hooks[o][r]=[]);var d=gform.hooks[o][r];null==n&&(n=r+”_”+d.length),gform.hooks[o][r].push(tag:n,callable:e,priority:t=null==t?10:t),doHook:function(r,o,e)var t;if(e=Array.prototype.slice.call(e,1),null!=gform.hooks[r][o]&&((o=gform.hooks[r][o]).sort(function(o,r)return o.priority-r.priority),o.forEach(function(o)”function”!=typeof(t=o.callable)&&(t=window[t]),”action”==r?t.apply(null,e):e[0]=t.apply(null,e))),”filter”==r)return e[0],removeHook:function(o,r,t,n)var e;null!=gform.hooks[o][r]&&(e=(e=gform.hooks[o][r]).filter(function(o,r,e)null!=t&&t!=o.priority)),gform.hooks[o][r]=e));

-
N/AFix spelling/grammar issueAdd or fix a linkAdd or fix an imageAdd more detailImprove the quality of the writingFix a factual error
-
You don’t need to tell us which article this feedback relates to, as we automatically capture that information for you.
-
This allows us to get in touch for more details if required.
-
Enter a five letter word in lowercase
#gform_wrapper_38 .gform_footer visibility: hidden; position: absolute; left: -100vw;
-
This field is for validation purposes and should be left unchanged.
/* = 0;if(!is_postback)return;var form_content = jQuery(this).contents().find(‘#gform_wrapper_38’);var is_confirmation = jQuery(this).contents().find(‘#gform_confirmation_wrapper_38’).length > 0;var is_redirect = contents.indexOf(‘gformRedirect(){‘) >= 0;var is_form = form_content.length > 0 && ! is_redirect && ! is_confirmation;var mt = parseInt(jQuery(‘html’).css(‘margin-top’), 10) + parseInt(jQuery(‘body’).css(‘margin-top’), 10) + 100;if(is_form)jQuery(‘#gform_wrapper_38’).html(form_content.html());if(form_content.hasClass(‘gform_validation_error’))jQuery(‘#gform_wrapper_38’).addClass(‘gform_validation_error’); else jQuery(‘#gform_wrapper_38’).removeClass(‘gform_validation_error’);setTimeout( function() /* delay the scroll by 50 milliseconds to fix a bug in chrome */ jQuery(document).scrollTop(jQuery(‘#gform_wrapper_38’).offset().top – mt); , 50 );if(window[‘gformInitDatepicker’]) gformInitDatepicker();if(window[‘gformInitPriceFields’]) gformInitPriceFields();var current_page = jQuery(‘#gform_source_page_number_38’).val();gformInitSpinner( 38, ‘https://geekymedics.com/wp-content/plugins/gravityforms/images/spinner.svg’, true );jQuery(document).trigger(‘gform_page_loaded’, [38, current_page]);window[‘gf_submitting_38’] = false;else if(!is_redirect)var confirmation_content = jQuery(this).contents().find(‘.GF_AJAX_POSTBACK’).html();if(!confirmation_content)confirmation_content = contents;jQuery(‘#gform_wrapper_38’).replaceWith(confirmation_content);jQuery(document).scrollTop(jQuery(‘#gf_38’).offset().top – mt);jQuery(document).trigger(‘gform_confirmation_loaded’, [38]);window[‘gf_submitting_38’] = false;wp.a11y.speak(jQuery(‘#gform_confirmation_message_38’).text());elsejQuery(‘#gform_38’).append(contents);if(window[‘gformRedirect’]) gformRedirect();jQuery(document).trigger(“gform_pre_post_render”, [ formId: “38”, currentPage: “current_page”, abort: function() this.preventDefault(); ]); if (event && event.defaultPrevented) return; const gformWrapperDiv = document.getElementById( “gform_wrapper_38” ); if ( gformWrapperDiv ) const visibilitySpan = document.createElement( “span” ); visibilitySpan.id = “gform_visibility_test_38”; gformWrapperDiv.insertAdjacentElement( “afterend”, visibilitySpan ); const visibilityTestDiv = document.getElementById( “gform_visibility_test_38” ); let postRenderFired = false; function triggerPostRender() if ( postRenderFired ) return; postRenderFired = true; jQuery( document ).trigger( ‘gform_post_render’, [38, current_page] ); gform.utils.trigger( event: ‘gform/postRender’, native: false, data: formId: 38, currentPage: current_page ); gform.utils.trigger( event: ‘gform/post_render’, native: false, data: formId: 38, currentPage: current_page ); if ( visibilityTestDiv ) visibilityTestDiv.parentNode.removeChild( visibilityTestDiv ); function debounce( func, wait, immediate ) var timeout; return function() var context = this, args = arguments; var later = function() timeout = null; if ( !immediate ) func.apply( context, args ); ; var callNow = immediate && !timeout; clearTimeout( timeout ); timeout = setTimeout( later, wait ); if ( callNow ) func.apply( context, args ); ; const debouncedTriggerPostRender = debounce( function() triggerPostRender(); , 200 ); if ( visibilityTestDiv && visibilityTestDiv.offsetParent === null ) const observer = new MutationObserver( ( mutations ) => mutations.forEach( ( mutation ) => if ( mutation.type === ‘attributes’ && visibilityTestDiv.offsetParent !== null ) debouncedTriggerPostRender(); observer.disconnect(); ); ); observer.observe( document.body, attributes: true, childList: false, subtree: true, attributeFilter: [ ‘style’, ‘class’ ], ); else triggerPostRender(); } );} );
/* ]]> */

Measuring and recording neurological observations and calculating a Glasgow Coma Scale (GCS) score can appear in OSCEs. You’ll be expected to correctly record neurological observations, record the findings and calculate a GCS score.
Indications
Neurological observations are undertaken in addition to, rather than replacing, National Early Warning Score 2 (NEWS2) basic observations. Neurological observations are most commonly undertaken in patients with a known or suspected primary neurological condition. They may also be monitored when a patient’s neurological function is affected to establish a baseline, inform patient management, and provide timely recognition of further deterioration.1-4
Indications include, but are not limited to:
- Suspected or confirmed head injury
- Suspected or confirmed cerebral vascular accident (CVA), intracerebral or subarachnoid haemorrhage
- Unexplained reduced level of consciousness
- Post-seizure
- Post-intervention, such as neurosurgical procedures or thrombolysis/thrombectomy
- Acute illness with no apparent cause
Gather equipment
Gather the relevant equipment for neurological observations:
- Pen torch
- Neurological observation chart


Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language.
Gain consent to proceed with recording neurological observations.
Ask if the patient has any pain before proceeding.
Introduction with reduced consciousness
Introductions depend on the patient’s current level of consciousness and may require differing approaches. For example, the patient may not be able to verbally confirm their name or date of birth, so this may be reliant on other identifiers, such as a hospital wristband. If the patient cannot give informed consent, neurological observations can be undertaken if deemed in the patient’s best interests.
Glasgow Coma Scale (GCS)
The GCS assesses patient responsiveness/consciousness level and commonly forms the basis of neurological observations. It differs from the ACVPU scale used in NEWS2 as a more detailed measurement of neurological function. The GCS assessment comprises of 3 components. Each component is assessed with the aim of gaining the best possible response from the patient, with each component assigned a score depending on the response elicited:1-3
- Eyes (score of 1-4)
- Verbal (score of 1-5)
- Motor (score of 1-6)
Non testable components
Other factors may affect the patient’s ability to provide an appropriate response for each GCS component. If additional limiting factors are present, the component is deemed not testable and recorded as NT rather than assigned a numerical value.
Appropriate use of physical stimulus
To elicit a response, the assessor may be required to apply a physical stimulus. Historically, this was referred to as assessing a response ‘to pain’; however, this is now commonly termed as assessing a response ‘to physical stimulus’ or ‘to pressure stimulus’ to better define the test being undertaken. This aims to assess the response to a temporary uncomfortable pressure stimulus rather than inflicting pain/injury. Therefore, only clinically appropriate forms of physical stimulus may be used.1
Most commonly used methods include:
- Fingertip pressure: applying pressure to the nail bed
- Trapezius squeeze/pinch: applying pressure over the trapezius muscle
- Supraorbital pressure: applying pressure to the supraorbital notch along the eyebrow ridge. Contraindicated in patients with facial trauma
Eye-opening response (E)
Opening spontaneously (4 points)
To assess eye response, initially observe if the patient opens their eyes spontaneously.
If the patient opens their eyes spontaneously, the assessment of eyes is complete, scoring 4 points.
If the patient does not open their eyes spontaneously, work through the following steps until a response is obtained.
Opening to sound (3 points)
If the patient doesn’t open their eyes spontaneously, speak to the patient, “Hi, Mrs Smith, can you open your eyes?”
If the patient’s eyes open in response to the sound of your voice, score 3 points.
Opening to pain (2 points)
If the patient’s eyes open in response to a physical stimulus, score 2 points.
No response (1 point)
If the patient does not open their eyes to a physical stimulus, score 1 point.
Not testable (NT)
If the patient cannot open their eyes for some reason (e.g. oedema, trauma, dressings), document that eye response could not be assessed (NT).
Summary
| Criterion | Score |
| Eye-opening spontaneously | 4 points |
| Eye-opening to sound | 3 points |
| Eye-opening to pain | 2 points |
| No response | 1 point |
| Not testable | NT |
Verbal response (V)
Assessing a patient’s verbal response initially involves engaging the patient in conversation and determining whether the patient is orientated to time and place.
Some common questions you can ask to help assess this might include:
- “Can you tell me your name?”
- “Do you know where you are at the moment?”
- “Do you know what the date is today?”
Orientated (5 points)
If the patient can answer questions appropriately and is orientated, the assessment of verbal response is complete, scoring 5 points.
Confused (4 points)
If the patient can communicate coherently but is confused (e.g. they don’t know where they are or what the date is), score 4 points.
Sometimes, confusion can be quite subtle, so pay close attention to their responses.
Inappropriate word (3 points)
If the patient can verbalise single, recognisable words that are unrelated to the question asked, score 3 points.
Inappropriate sounds (2 points)
If the patient can verbalise sounds, rather than speaking words (e.g. moans, groans), score 2 points.
No response (1 point)
If the patient has no response to your questions, they would score 1 point.
Not testable (NT)
If the patient is intubated or has other factors interfering with their ability to communicate verbally, their response cannot be tested, and for this, document NT.
Summary
| Criterion | Score |
| Orientated | 5 points |
| Confused | 4 points |
| Inappropriate words | 3 points |
| Incomprehensible sounds | 2 points |
| No response | 1 point |
| Not testable | NT |
Motor response (M)
Score the patient based on the highest scoring response you are able to elicit in any single limb (e.g. if they were unable to move their right arm, but able to obey commands with their left arm, they’d receive a score of 6 points).
Obeys commands (6 points)
Ask the patient to perform a two-part request (e.g. “Lift your right arm off the bed and make a fist.”).
If they follow this command correctly, score 6 points.
If the patient cannot obey commands, apply an appropriate physical stimulus and observe their response.
Localises to pain (5 points)
If the patient brings their hand(s) above their clavicle and attempts to reach the site at which you are applying a physical stimulus (e.g. head, neck), score 5 points.
Withdraws to pain (4 points)
If the patient tries to withdraw from the stimulus (e.g. pulls their arm away from you when applying a physical stimulus to their fingertip), score 4 points.
This is a normal flexion response, as this typically involves rapid flexion at the elbow to move away from the physical stimulus.
It differs from abnormal flexion to pain due to the absence of the other features mentioned below (e.g. internal rotation of the shoulder, pronation of the forearm, wrist flexion).
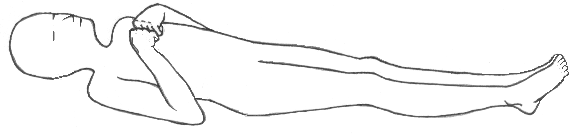
Abnormal flexion to pain (3 points)
Abnormal flexion to a physical stimulus typically involves adduction of the arm, internal rotation of the shoulder, flexion of the elbow, pronation of the forearm and wrist flexion (decorticate posturing), and scores 3 points.
Decorticate posturing indicates that significant damage may be present in the cerebral hemispheres, the internal capsule, and the thalamus.
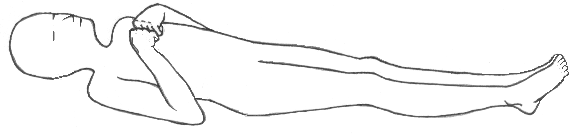
Abnormal extension to pain (2 points)
Abnormal extension to a physical stimulus typically involves the extension of the head and the extension and internal rotation of the arms and legs (decerebrate posturing), and scores 2 points.
This can be on just one side of the body or both (the signs may only be present in the upper limbs).
Decerebrate posturing indicates brain stem damage. It is exhibited by people with lesions or compression in the midbrain and lesions in the cerebellum. Progression from decorticate posturing to decerebrate posturing often indicates uncal (transtentorial) or tonsilar brain herniation (coning).


No response (1 point)
The complete absence of a motor response to a physical stimulus scores 1 point.
Not testable (NT)
If the patient is unable to provide a motor response (e.g. paralysis), document as not testable (NT).
Summary
| Criterion | Score |
| Obeys command | 6 points |
| Localises to pain | 5 points |
| Withdraws to pain | 4 points |
| Abnormal flexion to pain (decorticate) | 3 points |
| Abnormal extension to pain (decerebrate) | 2 points |
| No response | 1 point |
| Not testable | NT |
Summary of GCS criteria
Scores for each component are combined to give an overall score. Patients may score a minimum of 3/15, the lowest possible level of consciousness, and a maximum of 15/15, fully conscious.
The GCS should be documented, showing the score for each behaviour tested, e.g. GCS 15 [E4, V5, M6].

Limb movements
The motor response tested in the motor component of the GCS is further broken down into the movement observed in each limb. This helps compare and contrast neurological impairment between the left and right sides and between the upper and lower limbs.
Commonly, the NP-NM tool is used to assess limb movement, with each limb being measured against the following criteria:6
- Normal power
- Mild weakness
- Severe weakness
- Spastic flexion (arms only)
- Extension
- No response
Pupil reactions
Assess pupils for size, shape, and symmetry. Pupils should usually be circular and symmetrical. Typical pupil size varies between 2 and 5 mm.
The pupillary light reflex is tested by applying a light stimulus to the pupil, usually a pen torch. Both pupils should briskly constrict equally in response to light. This should be tested in both eyes. In health, both pupils should constrict regardless of which eye the light is being shone into. The pupil where the light stimulus is being applied constricts due to the direct reflex, while the other pupil constricts due to the consensual reflex.5
Pupil response should be recorded as normal (+), sluggish (S), no reaction (-), or closed by swelling (C).
Recording neurological observations
The measured observations should be recorded on a neurological observations chart, and the appropriate action should be taken based on the findings.
To complete the assessment…
Explain to the patient that the assessment is now complete.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
References
- Royal College of Physicians and Surgeons of Glasgow. The Glasgow Structured Approach to Assessment of the Glasgow Coma Scale. Published in n.d. Available from: [LINK]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974; 304:(7872)81-84. Available from: [LINK]
- Jain S, Iverson LM. Glasgow Coma Scale. 2023 Available from: [LINK]
- National Institute for Health and Care Excellence (NICE). Head injury: assessment and early management. NICE guideline [NG232]. 2023. Available from: [LINK]
- Belliveau AP, Somani AN, Dossani RH. Pupillary Light Reflex. 2023. Available from: [LINK]
- Cook NF, Braine ME, O’Rourke C, Nolan S. Assessment of motor limb strength by neuroscience nurses: variations in practice and associated challenges. British Journal of Nursing. 2022. 31(20). Available from: [LINK]
Image references
- Figure 1. EM3. Neurological observations chart. Adapted by Geeky Medics. License: [CC BY-NC-SA 4.0]. Available from: [LINK].
Discover more from Bibliobazar Digi Books
Subscribe to get the latest posts sent to your email.




