Suggest an improvement
var gform;gform||(document.addEventListener(“gform_main_scripts_loaded”,function()gform.scriptsLoaded=!0),document.addEventListener(“gform/theme/scripts_loaded”,function()gform.themeScriptsLoaded=!0),window.addEventListener(“DOMContentLoaded”,function()gform.domLoaded=!0),gform=domLoaded:!1,scriptsLoaded:!1,themeScriptsLoaded:!1,isFormEditor:()=>”function”==typeof InitializeEditor,callIfLoaded:function(o)(gform.isFormEditor()&&console.warn(“The use of gform.initializeOnLoaded() is deprecated in the form editor context and will be removed in Gravity Forms 3.1.”),o(),0)),initializeOnLoaded:function(o),hooks:action:,filter:,addAction:function(o,r,e,t)gform.addHook(“action”,o,r,e,t),addFilter:function(o,r,e,t)gform.addHook(“filter”,o,r,e,t),doAction:function(o)gform.doHook(“action”,o,arguments),applyFilters:function(o)return gform.doHook(“filter”,o,arguments),removeAction:function(o,r)gform.removeHook(“action”,o,r),removeFilter:function(o,r,e)gform.removeHook(“filter”,o,r,e),addHook:function(o,r,e,t,n)null==gform.hooks[o][r]&&(gform.hooks[o][r]=[]);var d=gform.hooks[o][r];null==n&&(n=r+”_”+d.length),gform.hooks[o][r].push(tag:n,callable:e,priority:t=null==t?10:t),doHook:function(r,o,e)var t;if(e=Array.prototype.slice.call(e,1),null!=gform.hooks[r][o]&&((o=gform.hooks[r][o]).sort(function(o,r)return o.priority-r.priority),o.forEach(function(o)”function”!=typeof(t=o.callable)&&(t=window[t]),”action”==r?t.apply(null,e):e[0]=t.apply(null,e))),”filter”==r)return e[0],removeHook:function(o,r,t,n)var e;null!=gform.hooks[o][r]&&(e=(e=gform.hooks[o][r]).filter(function(o,r,e)),gform.hooks[o][r]=e));

-
N/AFix spelling/grammar issueAdd or fix a linkAdd or fix an imageAdd more detailImprove the quality of the writingFix a factual error
-
You don’t need to tell us which article this feedback relates to, as we automatically capture that information for you.
-
This allows us to get in touch for more details if required.
-
Enter a five letter word in lowercase
#gform_wrapper_38 .gform_footer visibility: hidden; position: absolute; left: -100vw;
-
This field is for validation purposes and should be left unchanged.
/* = 0;if(!is_postback)return;var form_content = jQuery(this).contents().find(‘#gform_wrapper_38’);var is_confirmation = jQuery(this).contents().find(‘#gform_confirmation_wrapper_38’).length > 0;var is_redirect = contents.indexOf(‘gformRedirect(){‘) >= 0;var is_form = form_content.length > 0 && ! is_redirect && ! is_confirmation;var mt = parseInt(jQuery(‘html’).css(‘margin-top’), 10) + parseInt(jQuery(‘body’).css(‘margin-top’), 10) + 100;if(is_form)jQuery(‘#gform_wrapper_38’).html(form_content.html());if(form_content.hasClass(‘gform_validation_error’))jQuery(‘#gform_wrapper_38’).addClass(‘gform_validation_error’); else jQuery(‘#gform_wrapper_38’).removeClass(‘gform_validation_error’);setTimeout( function() /* delay the scroll by 50 milliseconds to fix a bug in chrome */ jQuery(document).scrollTop(jQuery(‘#gform_wrapper_38’).offset().top – mt); , 50 );if(window[‘gformInitDatepicker’]) gformInitDatepicker();if(window[‘gformInitPriceFields’]) gformInitPriceFields();var current_page = jQuery(‘#gform_source_page_number_38’).val();gformInitSpinner( 38, ‘https://geekymedics.com/wp-content/plugins/gravityforms/images/spinner.svg’, true );jQuery(document).trigger(‘gform_page_loaded’, [38, current_page]);window[‘gf_submitting_38’] = false;else if(!is_redirect)var confirmation_content = jQuery(this).contents().find(‘.GF_AJAX_POSTBACK’).html();if(!confirmation_content)confirmation_content = contents;jQuery(‘#gform_wrapper_38’).replaceWith(confirmation_content);jQuery(document).scrollTop(jQuery(‘#gf_38’).offset().top – mt);jQuery(document).trigger(‘gform_confirmation_loaded’, [38]);window[‘gf_submitting_38’] = false;wp.a11y.speak(jQuery(‘#gform_confirmation_message_38’).text());elsejQuery(‘#gform_38’).append(contents);if(window[‘gformRedirect’]) gformRedirect();jQuery(document).trigger(“gform_pre_post_render”, [ formId: “38”, currentPage: “current_page”, abort: function() this.preventDefault(); ]); if (event && event.defaultPrevented) return; const gformWrapperDiv = document.getElementById( “gform_wrapper_38” ); if ( gformWrapperDiv ) const visibilitySpan = document.createElement( “span” ); visibilitySpan.id = “gform_visibility_test_38”; gformWrapperDiv.insertAdjacentElement( “afterend”, visibilitySpan ); const visibilityTestDiv = document.getElementById( “gform_visibility_test_38” ); let postRenderFired = false; function triggerPostRender() if ( postRenderFired ) return; postRenderFired = true; jQuery( document ).trigger( ‘gform_post_render’, [38, current_page] ); gform.utils.trigger( event: ‘gform/postRender’, native: false, data: formId: 38, currentPage: current_page ); gform.utils.trigger( event: ‘gform/post_render’, native: false, data: formId: 38, currentPage: current_page ); if ( visibilityTestDiv ) visibilityTestDiv.parentNode.removeChild( visibilityTestDiv ); function debounce( func, wait, immediate ) var timeout; return function() var context = this, args = arguments; var later = function() timeout = null; if ( !immediate ) func.apply( context, args ); ; var callNow = immediate && !timeout; clearTimeout( timeout ); timeout = setTimeout( later, wait ); if ( callNow ) func.apply( context, args ); ; const debouncedTriggerPostRender = debounce( function() triggerPostRender(); , 200 ); if ( visibilityTestDiv && visibilityTestDiv.offsetParent === null ) const observer = new MutationObserver( ( mutations ) => mutations.forEach( ( mutation ) => if ( mutation.type === ‘attributes’ && visibilityTestDiv.offsetParent !== null ) debouncedTriggerPostRender(); observer.disconnect(); ); ); observer.observe( document.body, attributes: true, childList: false, subtree: true, attributeFilter: [ ‘style’, ‘class’ ], ); else triggerPostRender(); } );} );
/* ]]> */

Introduction
Learning how to interpret CT head scans can be challenging. A systematic approach ensures you do not miss any pathology.
In OSCEs, certain CT head findings and abnormalities commonly appear. You must be able to recognise these findings and discuss the management of these conditions.
These scans may appear as part of data interpretation stations, ABCDE/simulation stations and communication stations.
Ischaemic stroke
Ischaemic stroke occurs when the blood supply to an area of brain tissue is reduced, resulting in tissue hypoperfusion. The most common mechanisms are local thrombosis, embolism or systemic hypoperfusion (e.g. in cardiac arrest).
Patients will present with sudden onset neurological symptoms. Exact symptoms will vary depending on the area of infarction but may include slurred speech, reduced Glasgow coma score (GCS), limb weakness, sensory disturbance, visual changes and ataxia.
The primary role of a non-contrast CT head in suspected ischaemic stroke is to exclude haemorrhage. The appearance will vary depending on the duration between the onset time and CT scan, but includes:
- A normal scan: in the hyperacute phase (first few hours)
- Areas of hypodensity: representing ischaemia
- Hyperdense artery sign: dense thrombotic material in a cerebral artery (most commonly middle cerebral artery)
- Cerebral oedema
Management of ischaemic stroke
The immediate management of ischaemic stroke depends on the time from symptom onset and the local services available. Once non-contrast CT head excludes haemorrhage, high-dose aspirin (300 mg daily) should be prescribed immediately.
Thrombolysis is indicated if presenting within 4.5 hours of symptom onset (this may be extended in some situations). If available and CT angiography shows a suitable thrombus, thrombectomy may be carried out.
Patients require admission to an acute stroke unit for ongoing multidisciplinary team (MDT) management. This includes managing aspiration risk with speech and language therapy (SALT), blood glucose control, physiotherapy and occupational therapy, intermittent pneumatic compression devices for venous thromboembolism prophylaxis, treatment of any complications (e.g. aspiration pneumonia) and long-term modification of risk factors.
For further information, see the Geeky Medics guide to stroke.
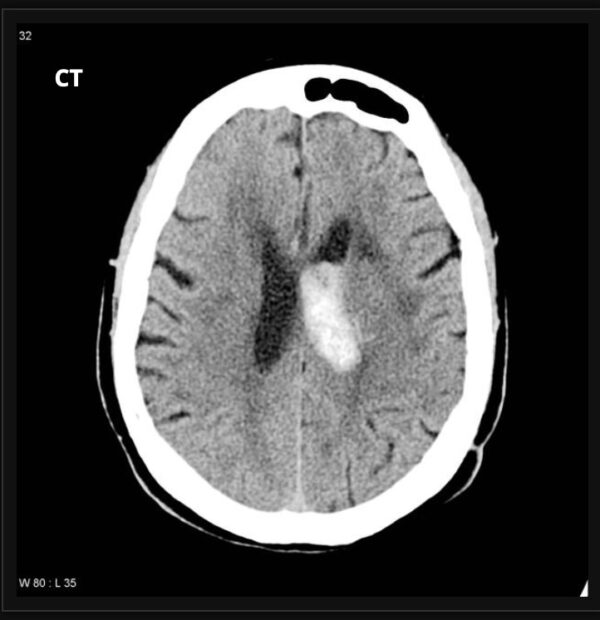
Haemorrhagic stroke
A haemorrhagic stroke, or intracerebral haemorrhage (ICH), involves bleeding from a ruptured blood vessel. Depending on the exact location, it can be intraparenchymal (within the brain tissue) and/or intraventricular (within the ventricles). They typically occur due to small vessel disease but may also result from haemorrhagic transformation of an ischaemic stroke.
Patients will present with sudden onset neurological symptoms, which will vary according to the blood vessel which ruptures but may include slurred speech, reduced GCS, limb weakness, sensory disturbance, visual changes and ataxia.
Features of ICH on CT head include:
- Hyperdensity within brain parenchyma or ventricles
- Anatomical location is dependent on the blood vessels affected
Management of haemorrhagic stroke
The immediate medical management of haemorrhagic stroke consists of anticoagulant reversal and blood pressure control (a degree of hypotension may be permitted) to prevent further expansion of the bleeding. Depending on the severity of the bleeding and the patient’s background, neurosurgical intervention may be required.
All patients should be admitted to an acute stroke unit for ongoing multidisciplinary team (MDT) management. This includes managing aspiration risk with speech and language therapy (SALT), blood glucose control, physiotherapy and occupational therapy, intermittent pneumatic compression devices for venous thromboembolism prophylaxis, treatment of any complications (e.g. aspiration pneumonia) and long-term modification of risk factors. Strict blood pressure control (systolic BP <150 mmHg) is required for the first 7 days.
For further information, see the Geeky Medics guide to stroke.
Extradural haematoma
An extradural haematoma (EDH) is an acute haemorrhage between the dura mater and the skull. Most are due to rupture of the middle meningeal artery (MMA) below the pterion due to trauma.
Patients typically experience an immediate loss of consciousness and a period of lucidity, followed by a progressive decline over a few hours. Other clinical features may include confusion, headache, nausea, vomiting, cranial nerve deficits, or upper motor neuron syndrome.
Features of EDH on CT head include:
- Bi-convex ‘lemon-shaped’ hyperdense mass
- Bleeding limited by sutures (i.e. the bleed will not cross the suture lines of the skull)
- Midline shift
- Brainstem herniation
Management of an extradural haematoma
Initial assessment of a patient with a suspected EDH should always follow an ABCDE approach. After this, the management will depend on several factors.
All patients on anticoagulants should receive reversal agents (e.g. vitamin K for warfarin), and any coagulopathy should be discussed with haematology. These patients are also at an increased risk of seizures, which should be managed appropriately with anticonvulsants if needed.
If a patient has raised intracranial pressure (ICP), they may be given intravenous mannitol, temporarily reducing the ICP while awaiting definitive management.
Definitive management will depend on the location and size of the bleed, the clinical features and the patient’s background, and may consist of:
- Monitoring: if the bleed is very small with minimal mass effect
- Burr hole craniotomy: in acute EDH, allowing evacuation of the haematoma
- Trauma craniotomy: in acute EDH with significant mass effect to evacuate blood, treat the cause of bleeding and reduce ICP
Subdural haematoma
A subdural haematoma (SDH) is a haemorrhage between the dura mater and the arachnoid mater. The bleeding typically comes from the rupture of the bridging cranial veins after a blow to the temporal side of the head. An SDH can be acute, subacute or chronic; this focuses on an acute SDH.
These bleeds are more common in older patients, those at increased risk of falls, and patients with coagulation abnormalities. Clinical features include headache, nausea, vomiting, and confusion. Patients can also present with drowsiness, which gradually worsens over the hours following the injury.
Features of acute SDH on CT head include:
- Crescent ‘banana-shaped’ hyperdense mass
- Bleeding not limited by sutures
- Midline shift
- Compression of ventricles
- Sulcal effacement (sulci appear less defined)
Management of a subdural haematoma
Initial assessment of a patient with a suspected SDH should always follow an ABCDE approach. After this, the management will depend on several factors.
All patients on anticoagulants should receive reversal agents (e.g. vitamin K for warfarin), and any coagulopathy should be discussed with haematology. These patients are also at an increased risk of seizures, which should be managed appropriately with anticonvulsants if needed.
Definitive management will depend on the location and size of the bleed, the clinical features and the patient’s background but may consist of:
- Monitoring: if the bleed is small with minimal mass effect
- Trauma craniotomy: the most common procedure for SDH, used to evacuate blood and reduce ICP
- Hemicraniectomy (depressive craniectomy): to prevent brainstem herniation in rising ICP
Some patients may be suitable for a burr hole craniotomy, but this is generally used in the management of chronic SDH rather than acute.
Subarachnoid haemorrhage
A subarachnoid haemorrhage (SAH) is a haemorrhage into the subarachnoid space between the arachnoid and pia mater. It is considered a subtype of haemorrhagic stroke. It is typically an arterial bleed and can be spontaneous or traumatic. Spontaneous SAHs are most commonly due to intracranial aneurysms or arteriovenous malformations (AVMs).
SAHs tend to present with a sudden onset, severe headache (thunderclap headache) and may have associated nausea, vomiting, photophobia, neck stiffness and reduced GCS.
Features of SAH on CT head include:
- Hyperdensity around the circle of Willis
- Hyperdensity in the subarachnoid space
A CT angiogram can be used to identify the presence of an aneurysm.
Management of a subarachnoid haemorrhage
The ABCDE approach should always be used for the initial assessment of a patient with a suspected SAH. These patients often have reduced GCS, so this should be assessed and monitored carefully, with consideration of anaesthetic input to manage the airway.
Once SAH has been confirmed, nimodipine (calcium channel blocker) is given to reduce cerebral artery spasm and reduce cerebral ischaemia. Patients should be discussed urgently with the local neurosurgical team for consideration of surgical intervention. They are at an increased risk of seizures, which should be managed appropriately with anticonvulsants if needed.
Surgical intervention may consist of:
- Obliteration of a ruptured aneurysm via clipping, insertion of a wire coil or other endovascular techniques
- Insertion of a ventricular drain
Editor
Dr Jamie Scriven
References
- Hellerhoff. Left middle cerebral artery stroke. Adapted by Geeky Medics. License: [CC BY-SA 3.0].
- Frank Gaillard. Radiopaedia.org, rID: 10598. Adapted by Geeky Medics. License: [CC BY-NC-SA 3.0]
- Hellerhoff. Epidural haematoma. Adapted by Geeky Medics. License: [CC BY-SA 3.0].
- James Heilman. Subdural haematoma. Adapted by Geeky Medics. License: [CC BY-SA 3.0].
- James Heilman. Spontaneous subarachnoid haemorrhage. Adapted by Geeky Medics. License: [CC BY-SA 3.0].
Discover more from Bibliobazar Digi Books
Subscribe to get the latest posts sent to your email.