Suggest an improvement
var gform;gform||(document.addEventListener(“gform_main_scripts_loaded”,function()gform.scriptsLoaded=!0),document.addEventListener(“gform/theme/scripts_loaded”,function()gform.themeScriptsLoaded=!0),window.addEventListener(“DOMContentLoaded”,function()gform.domLoaded=!0),gform=domLoaded:!1,scriptsLoaded:!1,themeScriptsLoaded:!1,isFormEditor:()=>”function”==typeof InitializeEditor,callIfLoaded:function(o)return!(!gform.domLoaded,initializeOnLoaded:function(o)gform.callIfLoaded(o),hooks:action:,filter:,addAction:function(o,r,e,t)gform.addHook(“action”,o,r,e,t),addFilter:function(o,r,e,t)gform.addHook(“filter”,o,r,e,t),doAction:function(o)gform.doHook(“action”,o,arguments),applyFilters:function(o)return gform.doHook(“filter”,o,arguments),removeAction:function(o,r)gform.removeHook(“action”,o,r),removeFilter:function(o,r,e)gform.removeHook(“filter”,o,r,e),addHook:function(o,r,e,t,n)null==gform.hooks[o][r]&&(gform.hooks[o][r]=[]);var d=gform.hooks[o][r];null==n&&(n=r+”_”+d.length),gform.hooks[o][r].push(tag:n,callable:e,priority:t=null==t?10:t),doHook:function(r,o,e)var t;if(e=Array.prototype.slice.call(e,1),null!=gform.hooks[r][o]&&((o=gform.hooks[r][o]).sort(function(o,r)return o.priority-r.priority),o.forEach(function(o)”function”!=typeof(t=o.callable)&&(t=window[t]),”action”==r?t.apply(null,e):e[0]=t.apply(null,e))),”filter”==r)return e[0],removeHook:function(o,r,t,n)var e;null!=gform.hooks[o][r]&&(e=(e=gform.hooks[o][r]).filter(function(o,r,e)null!=t&&t!=o.priority)),gform.hooks[o][r]=e));

-
N/AFix spelling/grammar issueAdd or fix a linkAdd or fix an imageAdd more detailImprove the quality of the writingFix a factual error
-
You don’t need to tell us which article this feedback relates to, as we automatically capture that information for you.
-
This allows us to get in touch for more details if required.
-
Enter a five letter word in lowercase
#gform_wrapper_38 .gform_footer visibility: hidden; position: absolute; left: -100vw;
-
This field is for validation purposes and should be left unchanged.
/* = 0;if(!is_postback)return;var form_content = jQuery(this).contents().find(‘#gform_wrapper_38’);var is_confirmation = jQuery(this).contents().find(‘#gform_confirmation_wrapper_38’).length > 0;var is_redirect = contents.indexOf(‘gformRedirect(){‘) >= 0;var is_form = form_content.length > 0 && ! is_redirect && ! is_confirmation;var mt = parseInt(jQuery(‘html’).css(‘margin-top’), 10) + parseInt(jQuery(‘body’).css(‘margin-top’), 10) + 100;if(is_form)jQuery(‘#gform_wrapper_38’).html(form_content.html());if(form_content.hasClass(‘gform_validation_error’))jQuery(‘#gform_wrapper_38’).addClass(‘gform_validation_error’); else jQuery(‘#gform_wrapper_38’).removeClass(‘gform_validation_error’);setTimeout( function() /* delay the scroll by 50 milliseconds to fix a bug in chrome */ jQuery(document).scrollTop(jQuery(‘#gform_wrapper_38’).offset().top – mt); , 50 );if(window[‘gformInitDatepicker’]) gformInitDatepicker();if(window[‘gformInitPriceFields’]) gformInitPriceFields();var current_page = jQuery(‘#gform_source_page_number_38’).val();gformInitSpinner( 38, ‘https://geekymedics.com/wp-content/plugins/gravityforms/images/spinner.svg’, true );jQuery(document).trigger(‘gform_page_loaded’, [38, current_page]);window[‘gf_submitting_38’] = false;else if(!is_redirect)var confirmation_content = jQuery(this).contents().find(‘.GF_AJAX_POSTBACK’).html();if(!confirmation_content)confirmation_content = contents;jQuery(‘#gform_wrapper_38’).replaceWith(confirmation_content);jQuery(document).scrollTop(jQuery(‘#gf_38’).offset().top – mt);jQuery(document).trigger(‘gform_confirmation_loaded’, [38]);window[‘gf_submitting_38’] = false;wp.a11y.speak(jQuery(‘#gform_confirmation_message_38’).text());elsejQuery(‘#gform_38’).append(contents);if(window[‘gformRedirect’]) gformRedirect();jQuery(document).trigger(“gform_pre_post_render”, [ formId: “38”, currentPage: “current_page”, abort: function() this.preventDefault(); ]); if (event && event.defaultPrevented) return; const gformWrapperDiv = document.getElementById( “gform_wrapper_38” ); if ( gformWrapperDiv ) const visibilitySpan = document.createElement( “span” ); visibilitySpan.id = “gform_visibility_test_38”; gformWrapperDiv.insertAdjacentElement( “afterend”, visibilitySpan ); const visibilityTestDiv = document.getElementById( “gform_visibility_test_38” ); let postRenderFired = false; function triggerPostRender() if ( postRenderFired ) return; postRenderFired = true; jQuery( document ).trigger( ‘gform_post_render’, [38, current_page] ); gform.utils.trigger( event: ‘gform/postRender’, native: false, data: formId: 38, currentPage: current_page ); gform.utils.trigger( event: ‘gform/post_render’, native: false, data: formId: 38, currentPage: current_page ); if ( visibilityTestDiv ) visibilityTestDiv.parentNode.removeChild( visibilityTestDiv ); function debounce( func, wait, immediate ) var timeout; return function() var context = this, args = arguments; var later = function() timeout = null; if ( !immediate ) func.apply( context, args ); ; var callNow = immediate && !timeout; clearTimeout( timeout ); timeout = setTimeout( later, wait ); if ( callNow ) func.apply( context, args ); ; const debouncedTriggerPostRender = debounce( function() triggerPostRender(); , 200 ); if ( visibilityTestDiv && visibilityTestDiv.offsetParent === null ) const observer = new MutationObserver( ( mutations ) => mutations.forEach( ( mutation ) => if ( mutation.type === ‘attributes’ && visibilityTestDiv.offsetParent !== null ) debouncedTriggerPostRender(); observer.disconnect(); ); ); observer.observe( document.body, attributes: true, childList: false, subtree: true, attributeFilter: [ ‘style’, ‘class’ ], ); else triggerPostRender(); } );} );
/* ]]> */

Introduction
This advanced life support (ALS) guide aims to provide an overview of the ALS guidelines and performing ALS in a hospital environment for cardiac arrest. It is based on the Resuscitation Council (UK) guidance and is intended only for students preparing for their OSCEs, not for patient care.
Advanced life support
Advanced life support (ALS) builds on basic life support (BLS) to provide patients with a higher level of care, increasing the likelihood of survival in the event of cardiac arrest.
To achieve this, ALS involves defibrillation, intravenous or intraosseous access, drugs, and advanced airway management. ALS is a team effort, and all parties must work together to provide the best possible outcome.
Anyone with the appropriate training can perform ALS, including doctors, nurses, paramedics, and other allied health professionals.
In-hospital cardiac arrest
When a collapsed patient is discovered in a hospital environment, a sequence of events should be followed to assess the situation. The initial assessment’s role is to confirm that the scene is safe to work in and then to identify the patient and their condition. It needs to be careful and quick to give the patient the best chance of survival.
Safety
While there are very few reports of harm to responders during resuscitation, ensuring the scene is safe is still essential.
For the environment to be safe, there should be a clear area around the patient to allow medical staff to work, and that environment needs to be free from hazards. If appropriate, move the patient to an open and safe area to allow 360° access, and patients on chairs should be moved onto the floor to allow for effective compressions.
Personal safety must also be maintained through personal protective equipment (PPE). This will normally include gloves and a type IIR facemask as a minimum, but may also include aprons, gowns, eye protection, and an FFP3 mask or respirator hood.
Please refer to your local hospital guidance regarding PPE/infection prevention measures.
Patient assessment
After checking safety and donning appropriate PPE, approach the patient and begin the assessment:
1. Assess their level of consciousness. Are they alert or responsive to a verbal or physical stimulus? If they are unresponsive to pain, they can be deemed to be unconscious
2. Open and assess the patient’s airway by using either a head-tilt chin-lift or jaw thrust
3. Look, listen, and feel for breathing and palpate the carotid artery for ten seconds
4. If there is ineffective breathing or no palpable pulse, confirm cardiac arrest and shout for help
5. Start basic life support at a ratio of 30 compressions to 2 ventilations until a defibrillator arrives
High-quality chest compressions
Chest compression should have:
- A depth of 5-6 cm
- A rate of 100-120 compressions per minute
Respiratory arrest
If the patient has a pulse but is not breathing (respiratory arrest), ventilate as above and continue to check for a pulse every minute. Treating the cause of respiratory arrest is essential as these patients will soon progress to cardiac arrest.
If at any point a pulse cannot be felt, then start chest compressions.
Monitored cardiac arrest
Sometimes, a patient may have a witnessed cardiac arrest while attached to cardiac monitoring in, for example, but not limited to the:
- Catheter laboratory
- Emergency department resus
- Coronary care unit
- Critical care unit
- Recovery unit after cardiac surgery
In these situations, a defibrillator is often rapidly available, and the following steps should be followed:
1. Confirm cardiac arrest and shout for help
2. Consider administering a precordial thump while accessing and attaching the defibrillator
3. If the initial rhythm is ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) give three quick shocks in succession
4. Check for a rhythm change and pulse
5. If the third shock is unsuccessful, then begin chest compressions and follow the ALS algorithm for ongoing management (in this situation, these three shocks are considered the first shock in the algorithm)
Early chest compressions
Early effective chest compressions and defibrillation are the first two steps in the chain of survival, so if at any point there is any doubt about signs of life or the presence of a pulse, begin chest compressions.
Any delays in commencing CPR can significantly reduce the chance of survival.
Defibrillation
Once cardiac arrest has been confirmed, the initial priority is early defibrillation.
Defibrillation
1. Continue basic life support at a ratio of 30:2
2. Attach defibrillator pads to the patient’s chest (as labelled)
3. Assess the rhythm and shock the patient if appropriate before continuing the ALS algorithm (see below)
4. Rhythm checks should be performed every two minutes, and rescuers performing CPR should be frequently swapped to prevent fatigue and maintain high-quality CPR
Defibrillator safety
When applying defibrillator pads, defibrillation safety should always be considered. To do this, consider the 6Ps:
- Perspiration: excessive perspiration should be dried to allow pad adhesion
- Pacemakers: defibrillation pads should not be placed over pacemakers
- Patches: defibrillation pads should not be placed over transdermal drug patches. The patches can be removed or pad placement altered
- Piercings: defibrillation pads should not be placed directly over body piercings
- Puddles: patients should be moved into a dry environment before defibrillation
- Explosive environments: for the safety of the patient and rescuers, defibrillation should not occur in a potentially explosive environment
Considering these factors when defibrillating a patient will prevent patient harm and maintain the safety of clinicians.
Before defibrillation, no staff or equipment must be touching the patient. CPR should be continued as the defibrillator is charged, and a full top-to-toe sweep should be completed. Eyes should be kept on the patient as the shock is delivered to ensure no one accidentally makes contact.
CPR should be restarted as soon as the shock is delivered, minimising time off the chest.
Manual defibrillation
To be responsible for the defibrillator in manual mode, a staff member should have completed ALS training.
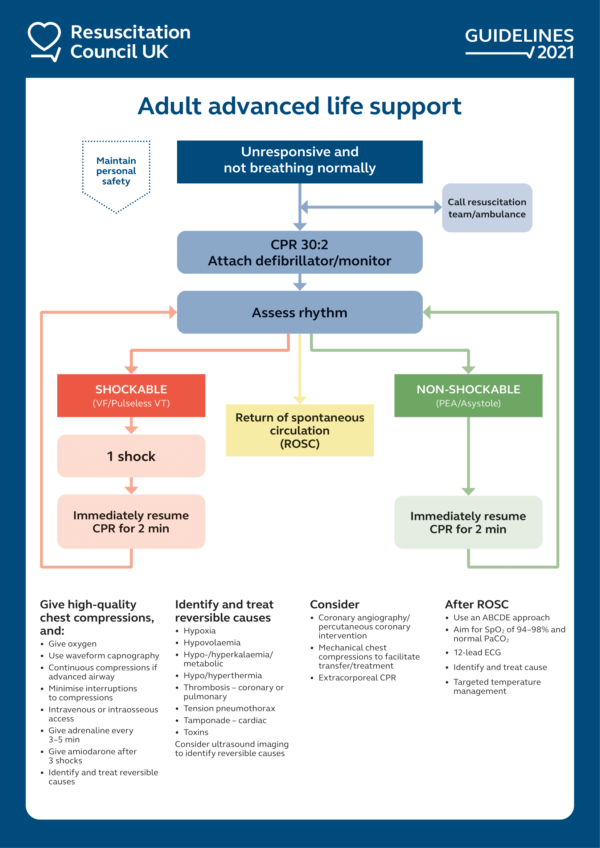
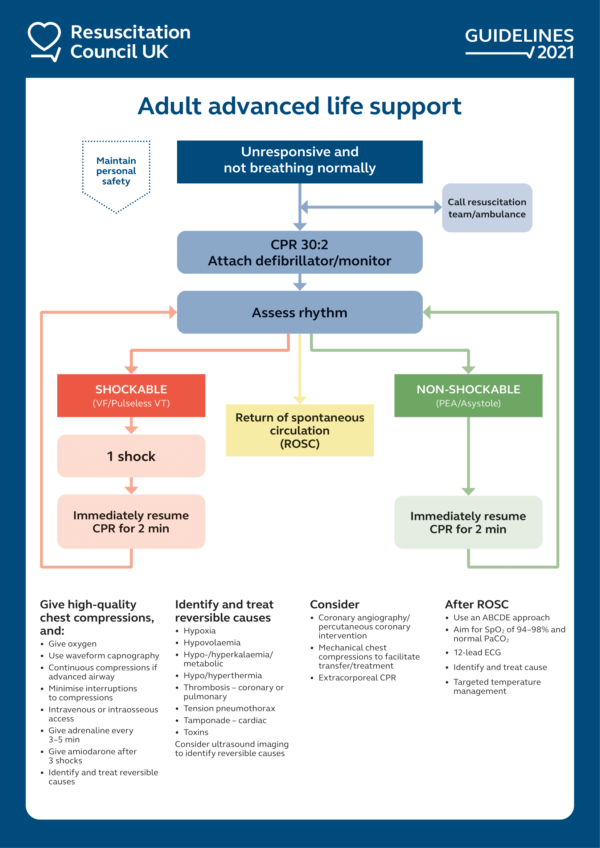
The ALS algorithm
ALS uses an algorithm with two distinct pathways to provide a systematic approach to managing cardiac arrest.
When following the ALS algorithm, it is important to remember the basics, with high-quality CPR and early defibrillation being the top priorities, quickly followed by gaining intravenous (IV)/intraosseous (IO) access and upgrading to an advanced airway.
Actions such as gaining IV/IO access, upgrading the airway, administering drugs and considering reversible causes should be completed during the two minutes of CPR.
There are two sides to the ALS algorithm: shockable and non-shockable.
Shockable rhythms
If the patient is in pulseless ventricular tachycardia (pVT) or ventricular fibrillation (VF) then the shockable algorithm should be followed.
1. If the initial rhythm is shockable, provide one shock (at the recommended joules for your equipment)
2. Immediately resume CPR for 2 minutes before performing another rhythm check
3. Increase the joules with each shock in line with your organisational guidance
4. After the third shock, administer 300 mg amiodarone and 1 mg adrenaline IV/IO
5. Continue to give adrenaline every 3-5 minutes
6. After the fifth shock, administer amiodarone 150 mg
7. Repeat until the return of spontaneous circulation (ROSC) is achieved or the patient moves into the non-shockable side of the algorithm
Tip: always check for a pulse and signs of life if the monitor shows VT, as this rhythm may be a pulsed, perfusing rhythm
Non-shockable rhythms
If the patient is in pulseless electrical activity (PEA), or asystole then the non-shockable algorithm should be used.
1. Immediately resume CPR for 2 minutes before performing another rhythm check
2. Administer adrenaline 1 mg IV/IO as soon as possible after identifying a non-shockable rhythm
3. Perform a pulse and rhythm check after every 2 minutes of CPR
4. Continue to give adrenaline every 3 – 5 minutes
5. Repeat until ROSC is achieved, or the patient moves into the shockable side of the algorithm
If the patient moves between shockable and non-shockable rhythms, once the adrenaline has been administered, it should be given every 3-5 minutes, regardless of the rhythm, until ROSC is achieved.
Documentation
One of the most important roles in an emergency is the scribe. Someone should always be assigned to document the actions of the cardiac arrest team, including event timings and medications administered.
Depending on the area of the emergency, your hospital may have a proforma that can be completed with this information (e.g. a critical interventions log in the emergency department).
Reversible causes of cardiac arrest
There are eight reversible causes of cardiac arrest, the four Hs and four Ts:
- Hypoxia
- Hypokalaemia/hyperkalaemia
- Hypothermia/hyperthermia
- Hypovolaemia
- Tension pneumothorax
- Tamponade (cardiac)
- Thrombosis
- Toxins
It is important to quickly identify and manage reversible causes during a cardiac arrest scenario. Successful management and reversal will increase the likelihood of ROSC.
The fact that death ends with T and H should prompt the four Hs and Ts.
Airway management
Airway management and airway protection are vital in cardiac arrest for appropriate ventilation and oxygenation.
A stepwise approach should be taken towards airway management, with manual techniques being used first, followed by more advanced equipment when appropriately trained staff arrive.
For more information on airway management devices, see the Geeky Medics guide to airway equipment.
Oropharyngeal airway
An oropharyngeal airway (OPA) should be used during the initial phases of a cardiac arrest as they are quick and easy to insert and work well with a bag-valve-mask for ventilation.
Nasopharyngeal airway
Nasopharyngeal airways (NPA) can be used in place of an OPA in the event of trismus or an obstruction in the mouth.
Supraglottic airway/i-gel®
Supraglottic airways are inserted into the pharynx, enabling higher-pressure ventilation and expiratory gas monitoring.
There are various supraglottic airways, including laryngeal mask airways (with either inflatable or silicone/rubber cuffs), and the i-gel® with a thermoplastic elastomer used to create a seal around the larynx.
The use of supraglottic airways is common in cardiac arrests due to their relatively simple insertion technique.
Endotracheal intubation
An endotracheal tube is guided through the larynx and into the trachea before an inflatable cuff seals the tube in its place. This allows for high-pressure ventilation and significantly reduces the risk of aspiration of stomach contents. Endotracheal intubation is a definitive airway but should only be placed by suitably trained staff, i.e. an anaesthetist.
When an advanced airway is in place, the correct placement must be confirmed by auscultation and measurement of end-tidal CO₂ via waveform capnography.
Rhythm recognition
One of the essential skills in ALS is cardiac rhythm recognition. This is crucial to help decide the correct course of treatment when following the ALS algorithm. Our article on ECG interpretation covers this in detail.
Types of monitoring
In an emergency, cardiac monitoring should be established as soon as possible. The main methods for monitoring cardiac rhythm are:
- ECG monitoring: a patient is attached to a cardiac monitor via adhesive electrodes, and the ECG is displayed on the screen in real-time. This is typically a three-lead ECG, using modified limb leads I, II and III. Modified lead II is most commonly used to identify arrhythmias, although others can be used if needed
- Emergency monitoring: in a collapsed patient, the defibrillator acts as a monitor once the defibrillator pads are attached. It typically displays modified lead II and allows rapid determination of rhythm
The ECG displays from these monitors should only be used for rhythm recognition, not for interpretation of other pathologies such as ST-segment elevation. If more detailed ECG interpretation is needed then a full twelve lead ECG should be obtained.

Peri-arrest arrhythmias
Cardiac arrhythmias occurring in the peri-arrest period can be split into two main categories:
1. Arrhythmias that may lead to cardiac arrest
2. Arrhythmias that may occur following initial resuscitation from cardiac arrest
Recognition and initial management of common arrhythmias found in these situations is essential knowledge to help manage or prevent cardiac arrest. Arrhythmias are generally classified by their heart rate:
- Tachyarrhythmias
- Bradyarrhythmias
- Arrhythmias with a normal heart rate
Most peri-arrest rhythms will fall into the tachy- or bradyarrhythmia categories. However, it is still important to be aware of other arrhythmias that may represent a risk of deterioration to cardiac arrest (e.g. hypokalaemia).
Management of peri-arrest arrhythmias
In all cases of arrhythmia, the first step should be to carry out an ABCDE assessment. One of the most important things to establish during this is whether any adverse features are present:
- Shock: hypotension (systolic blood pressure < 90 mmHg), sweating, pallor, cold extremities, increased capillary refill time, confusion
- Syncope
- Heart failure: pulmonary oedema, raised JVP
- Myocardial ischaemia: typical ischaemic chest pain, evidence of ischaemia on an ECG
These features suggest that a patient is unstable and, therefore, at risk of further deterioration, meaning more urgent interventions will be needed.
Extremes of heart rate
Extremes of heart rate may be considered an adverse feature at heart rates above 150 bpm and below 40 bpm due to their impact on cardiac output.
At heart rates above 150, diastole is significantly shortened, reducing cardiac filling (and therefore cardiac output) and blood flow to the coronary muscle.
During significant bradycardia, stroke volume needs to increase to compensate for this, which becomes much harder the slower the heart is beating, particularly if patients already have impaired cardiac function.
This initial assessment helps to guide the immediate treatment needed into one of the following options:
- No treatment
- Simple interventions, e.g. vagal manoeuvres
- Pharmacological management
- Electrical management: cardioversion for tachyarrhythmia or pacing for bradyarrhythmia
Tachyarrhythmias
For tachyarrhythmia with adverse features, the initial management is synchronised cardioversion. This should be carried out under conscious sedation or general anaesthesia.
Cardioversion is carried out via an attached defibrillator, and this should be set to deliver a synchronised shock, meaning that the shock will coincide with the R wave. If not synchronised, there is a risk of inducing VF.
The following process should be followed after identifying the need for synchronised cardioversion:
1. Ensure the defibrillator is set to deliver a synchronised shock
2. Ensure no staff or equipment are touching the patient
3. Select the correct joules for the shock depending on the rhythm and equipment: for broad complex tachycardia and atrial fibrillation, start with 120-150 J, and for narrow complex tachycardia and atrial flutter, start with 70-120 J
4. Press and hold the shock button on the defibrillator until the shock is delivered
5. If this fails to terminate the arrhythmia, prepare to deliver a second shock by repeating steps 1-4, but increase the joules in line with organisational guidance
A total of three shocks can be delivered during synchronised cardioversion. If, following this, the arrhythmia has not terminated or adverse features are still present, administer 300 mg amiodarone IV over 10-20 minutes.
Following this, further synchronised cardioversion can be attempted. This loading dose of amiodarone should be followed by an infusion over 24 hours of 900mg amiodarone, given into a large vein.


If there are no adverse features, then the arrhythmia should be assessed further and categorised based on the duration of the QRS complex.
Broad complex tachyarrhythmias
With a QRS duration ≥0.12s and includes:
- Ventricular tachycardia
- Supraventricular rhythm with bundle branch block
- Atrial fibrillation with bundle branch block
- Polymorphic ventricular tachycardia
Narrow complex tachyarrhythmias
With a QRS duration <0.12s and includes:
- Sinus tachycardia
- Atrioventricular nodal re-entry tachycardia (AVNRT)
- Atrioventricular re-entry tachycardia (AVRT): due to Wolff-Parkinson White (WPW) syndrome
- Atrial flutter
Bradyarrhythmias
For bradyarrhythmia with adverse features, the initial management is pharmacological measures. Administer 500 micrograms atropine IV, and if required, repeat every 3-5 minutes to a maximum of 3 mg (i.e. 6 doses).
Atropine should be used with caution in those with acute myocardial ischaemia or myocardial infarction, as the increase in heart rate may worsen ischaemia.
If initial pharmacological management with atropine fails to terminate the bradyarrhythmia and adverse signs are still present, or atropine is contraindicated, cardiac pacing is required. This should take the form of transcutaneous pacing initially, and advice should be sought on whether transvenous pacing is required.
In specific circumstances or as an interim measure, alternative medications include:
- IV isoprenaline infusion
- IV adrenaline infusion
- IV aminophylline: in inferior myocardial infarction, spinal cord injury or cardiac transplant patients
- IV glucagon: if the bradycardia is likely due to beta-blockers or calcium channel blockers
- IV dopamine infusion
If there are no adverse features present, then determine if the patient has a high risk of asystole:
- Recent asystole
- Mobitz type II AV block
- Complete heart block with broad QRS complexes
- Ventricular pauses > 3 seconds
If one of these features is present, manage as if adverse features are present with IV atropine and progression to second-line medications or cardiac pacing.


If there are no adverse features and the patient is not at high risk of asystole, immediate management is not needed, but further assessment should be conducted to investigate the cause of the bradycardia.
Blood gas analysis
Blood gas analysis is another essential skill in ALS and the ongoing management of resuscitated patients. In a cardiac arrest, an arterial blood gas (ABG) should be taken to assess the acid-base status, respiratory gas exchange and electrolytes.
Important values include:
- pH
- PaO2
- PaCO2
- Bicarbonate
- Base excess
- Lactate
- Potassium
- Haemoglobin
A VBG may be used in place of an ABG, but determination of gas exchange may be more difficult.
For further information, see the Geeky Medics guide to ABG interpretation.

Resuscitation in special circumstances
In certain cardiac arrest situations, the ALS algorithm is adapted to provide more specific treatment and increase the likelihood of survival.
Anaphylaxis
Anaphylaxis is a severe and life-threatening reaction to an antigen, presenting with rapid onset ABC impairment or significant skin/mucosal changes. It can cause global oedema, resulting in hypovolemia, as well as swelling to the airway, causing significant occlusion.
Early intramuscular adrenaline should be administered in a patient with suspected anaphylaxis. This will significantly reduce the likelihood of cardiac arrest.
Anaphylaxis leads to airway closure due to rapid swelling, causing hypoxia and hypovolemia due to anaphylactic shock. These should be managed as reversible causes of cardiac arrest.
Early intubation should be considered, as rapid airway swelling will make management increasingly difficult. In the event of complete airway occlusion, surgical intervention may be required.
The refractory anaphylaxis treatment algorithm may also be useful, as an adrenaline infusion may be required once ROSC is achieved.
For more information, see the Geeky Medics guide to anaphylaxis.
Asthma and COPD
Chronic obstructive pulmonary disease (COPD) and asthma are extremely common in the UK, with 1 in 5 people having lung disease. Patients with these conditions may experience acute exacerbations causing hypoxia, potentially leading to cardiac arrest.
The primary cause of cardiac arrest in COPD and asthma patients is hypoxia, either due to bronchospasm or mucous plugging. Consider early tracheal intubation due to increased intrathoracic pressure.
Provide manual ventilation over mechanical ventilation to reduce the risk of hyperinflation and barotrauma.
Monitor for signs of tension pneumothorax and treat with thoracostomy as appropriate.
For more information, see the Geeky Medics guides to the acute management of asthma and the acute management of COPD.
Drowning
In the UK, around 600 people die by drowning each year. Correctly managing a drowned patient is critical, as early intervention can increase survival.
Drowning causes respiratory failure through immersion or submersion. As such, the leading cause of cardiac arrest is hypoxia. However, hypothermia and arrhythmias should also be considered.
In water <5°C, hypothermia is likely to be the primary cause, providing some protection against hypoxia.
Palpation of a pulse is unreliable in cold and wet patients. Therefore, ECG and waveform capnography should be utilised to confirm cardiac arrest.
Give five rescue breaths before continuing standard ALS procedures. Consider early intubation, as pulmonary oedema may require high-pressure ventilation.
Hypo-/hyperkalaemia and electrolyte disturbances
Deranged electrolytes, particularly potassium, should be considered in all patients with an arrhythmia or cardiac arrest. Depending on the situation and whether the patient is currently in cardiac arrest, an ECG may be the most available diagnostic tool. Potassium levels can then be checked using point-of-care testing to guide initial management, with a further serum sample sent to the lab for confirmation.
For a patient in cardiac arrest with confirmed hyperkalaemia:
- Give 10 mL calcium chloride 10% IV to stabilise the cardiac myocytes
- Give 10 units insulin alongside 25 g glucose IV to shift potassium into cells
- Give 10% glucose infusion according to the blood glucose
- Consider 50 mmol sodium bicarbonate if metabolic acidosis to further shift potassium into cells
If hyperkalaemia is refractory, then dialysis should be considered.
For further information on the management of electrolyte disorders in cardiac arrest, see the Geeky Medics guide to reversible causes of cardiac arrest.
Hypothermia
Hypothermia occurs when the environment is too cold for a person’s body to regulate, and the core temperature drops. This decreases cerebral outflow and reduces cardiac output, resulting in cardiac arrest.
To confirm cardiac arrest, look, listen and feel for a pulse, ECG activity or breathing for up to one minute.
If the patient’s temperature is below 30°C and VF persists after three defibrillation attempts, withhold further shocks until their temperature rises above 30°C.
No cardiac arrest drugs should be given if the patient’s body temperature is below 30°C.
If the body temperature is 30-34°C, the timing of adrenaline intervals should be doubled to every 6-10 minutes.
All efforts should be made to rewarm the patient using conventional blankets, heat lamps, and warming air blankets.
Where possible, warm the patient via extracorporeal life support (ECLS) and extracorporeal membrane oxygenation (ECMO).
For further information on hypothermia and its management, see the Geeky Medics guide to reversible causes of cardiac arrest.
Maternal cardiac arrest
Pregnant women experience physiological changes, and their bodies are placed under additional stress. Whilst maternal cardiac arrests are relatively infrequent, the correct management is vital for patient survival. There are two patients, both of whom need to be rescued.
Maternal arrests are commonly caused by hypoxia or hypovolaemia. Consider the likelihood of concealed intrauterine bleeding.
Call for specialist help immediately, including obstetrics and neonatology. Consider early intubation to help manage the potentially oedematous airway.
If the patient is more than 20 weeks pregnant, the uterus should be displaced to the left lateral side. This will reduce aortocaval compression, potentially improving cardiac output.
If possible, apply left lateral tilt to the patient by angling the patient’s bed or using a ‘wedge’ block.
If ROSC is not achieved within four minutes of cardiac arrest, prepare for the emergency delivery of the fetus (resuscitative hysterotomy).
Obesity
With an increasingly obese population, it is important to recognise how to manage these patients in cardiac arrest situations.
The normal ALS algorithm should be followed. Chest compressions will be increasingly difficult, and rescuers should be swapped more frequently to prevent fatigue. Anticipate difficult intubation and airway management.
It may also be worth considering adjuncts like steps or adjusting bed heights and early use of mechanical chest compression devices.
Overdose
Intentional or accidental overdoses are becoming increasingly common, with potentially devastating effects.
Always maintain personal safety, especially if the cause is unknown or likely to be part of a CBRNE incident.
Use specific antidotes as appropriate (e.g. naloxone), and consult toxbase guidance where required.
Prolonged CPR may be appropriate for this cohort of patients, and a good neurological outcome is possible. Extracorporeal cardiopulmonary resuscitation (ECPR) may be appropriate.
For more information, see the Geeky Medics guides to benzodiazepine, opioid, salicylate, and tricyclic antidepressant overdose.
Opioid overdose
Of all drugs taken in overdose, opioids have been consistently shown to be the most likely to cause death. Respiratory arrest usually leads to cardiac arrest, with hypoxia as the primary reversible cause.
In opiate overdoses, naloxone can be administered:
- Provide an initial dose of 400 micrograms IV/IO
- Subsequent doses should be 800 micrograms IV/IO, every 60 seconds
- Doses should be titrated until the patient is breathing adequately and has protective airway reflexes
- If there has been no response after 10 mg of naloxone, another cause should be considered
- Naloxone administration should not compromise good quality CPR, early defibrillation, or airway management
For more information, see the Geeky Medics guide to the emergency management of an opioid overdose.
Perioperative cardiac arrest
Cardiac surgery
Cardiac surgery and its post-operative period carry a risk of cardiac arrest. In these cases, patients should be managed according to a modified ALS algorithm:
- Do not routinely give adrenaline during the arrest
- For VF/pVT, give 3 shocks via defibrillator in quick succession
- For asystole or extreme bradycardia, apply early transcutaneous pacing
- For PEA, try to correct any reversible causes. If the patient has a paced rhythm, then pacing should be stopped to exclude VF
If ROSC is not achieved after these initial steps, chest compressions and ventilation should be started, with early consideration of re-sternotomy and extracorporeal CPR.
Malignant hyperthermia
In the perioperative setting, patients may experience malignant hyperthermia, a severe reaction to inhaled anaesthetics and succinylcholine (muscle relaxant) that results in muscle rigidity, fever, tachycardia and acidosis. Without rapid intervention, this can progress to cardiac arrest.
Any triggering agent should be immediately stopped and oxygen administered, aiming to maintain normocapnia.
Dantrolene should be given to treat the malignant hyperthermia, and hyperkalaemia and acidosis managed accordingly.
Active cooling is generally necessary, and in cases of cardiac arrest, this should be continued alongside the ALS algorithm.
Sepsis
Sepsis is one of the leading causes of hospital admission, with patients being at high risk of deterioration into septic shock. When this occurs, blood pressure drops and body systems fail to receive sufficient oxygen, potentially causing cardiac arrest.
When managing a cardiac arrest due to sepsis, follow the standard ALS algorithm and provide a 500 mL fluid bolus as soon as possible.
For further information, see the Geeky Medics guide to the emergency management of sepsis.
Tamponade
Cardiac tamponade results from blood or fluid accumulating in the pericardial space. This limits the filling of the ventricles, reduces stroke volume and cardiac output, and causes cardiac arrest.
In cardiac arrest, the priority should be the identification of cardiac tamponade using point-of-care echocardiography and immediate decompression of the pericardium via resuscitative thoracotomy or pericardiocentesis.
For further information on the management of tamponade in cardiac arrest, see the Geeky Medics guide to reversible causes of cardiac arrest.
Tension pneumothorax
A tension pneumothorax is the continued collection of air in the pleural space, which compresses the structures in the chest (including the heart) and leads to haemodynamic compromise.
Clinical features of a tension pneumothorax include tracheal deviation, absent breath sounds (unilateral) and cyanosis.
In cardiac arrest, tension pneumothorax should be confirmed on clinical examination or with point-of-care ultrasound. Following this, the immediate priority should be decompression of the chest with needle decompression and/or thoracostomy. As decompression is the only effective treatment for tension pneumothorax it should take priority over other measures.
For further information on the management of tension pneumothorax in cardiac arrest, see the Geeky Medics guide to reversible causes of cardiac arrest.
Thrombosis
Pulmonary embolism
If pulmonary embolus is thought to be the cause of cardiac arrest, then thrombolytic therapy should be administered, and it may be appropriate to continue CPR for 60-90 minutes after this. In these cases, mechanical chest compression devices or extracorporeal CPR should be considered to reduce the risk of poor-quality chest compressions that may result from fatigue in extended resuscitation efforts.
Coronary thrombus
Occlusion of a coronary vessel with a thrombus will result in a myocardial infarction, which may then lead to cardiac arrest. In these situations, the priority is to identify the infarction and arrange primary percutaneous coronary intervention (PPCI) within 120 minutes, for reperfusion.
For further information on the management of thrombosis in cardiac arrest, see the Geeky Medics guide to reversible causes of cardiac arrest.
Traumatic cardiac arrest
Cardiac arrest in trauma is often due to a combination of hypovolaemic, obstructive and neurogenic shock, depending on the injuries sustained. A rapid response is essential, and patients should ideally be managed in a specialised trauma centre after focused pre-hospital care.
Management of cardiac arrest in trauma should focus on:
- Haemorrhage control: using external pressure, haemostatic gauze, tourniquets and pelvic binders
- Use of ultrasound to identify the cause of cardiac arrest
- Consideration of resuscitative thoracotomy
Chest compressions should not delay the treatment of any reversible causes of traumatic cardiac arrest.
Post-resuscitation care
Return of spontaneous circulation (ROSC) is when the heart sustains an electrical rhythm compatible with life and cardiac output following cardiac arrest. However, ongoing supportive treatment is needed to prevent repeated episodes of cardiac arrest.
If ROSC is achieved, a full ABCDE assessment should be undertaken. It is important to remember that the patient has a high risk of re-arresting and be prepared to intervene if necessary.
It is also essential to update the patient’s family after the emergency.
Airway
The majority of patients will require ongoing airway and ventilation support following ROSC. Those with a very brief period of cardiac arrest may not require tracheal intubation but should be given oxygen via a face mask to prevent hypoxia.
Breathing
Oxygen saturations should be maintained at 94 – 98% to prevent hypoxia or hyperoxia.
If the patient is breathing at a sustainable rate (above 10 breaths per minute), allow them to self-ventilate. If they are hypoventilating, assistance may be required, which can be via a bag-valve mask or, preferably, a mechanical ventilator.
Measure end-tidal CO₂ and aim for a capnography reading of 4.6 – 6.0 kPa, with a good waveform.
Circulation
Following a cardiac arrest, repeat 12-lead ECGs should be performed to highlight any significant changes (e.g. ST-segment elevation), and echocardiography should be considered to identify myocardial dysfunction.
Hypotension should be avoided, and the mean arterial pressure should be sufficient to maintain urine output >0.5 mL/kg/hr and a normal or decreasing lactate level. Fluids or inotropes may be necessary to achieve this in the period following ROSC.
Disability
Most patients will have a significantly reduced level of consciousness post-ROSC.
However, in some cases, they may become agitated and combative. In these situations, senior clinicians should be consulted to consider sedation or anaesthesia.
Some patients may experience seizures following cardiac arrest. These should be diagnosed using electroencephalography (EEG) and treated accordingly. Levetiracetam or sodium valproate are generally used as first-line treatments.
Exposure
The patient’s temperature should be measured and appropriately managed to prevent fever for at least 72 hours following ROSC.
Ongoing treatment
Once ROSC has been achieved and the patient is stable enough to move, they should be transferred to a higher-care area, depending on their particular treatment needs, such as the intensive care unit (ICU) or coronary care unit (CCU).
Depending on the possible cause of the cardiac arrest, investigations such as a chest X-ray, coronary angiography, or CT scan (most commonly CT head or CT pulmonary angiography) should be arranged.
Alongside treating any identified cause for the cardiac arrest, ongoing treatment should include:
- Aim to maintain temperature <37.7°C for 72 hours
- Maintain oxygen saturation 94 – 98%
- Optimising fluid status
- Blood glucose monitoring and control: the priority is to avoid hypoglycaemia
- Monitor for any seizures
- Initiating any necessary secondary prevention, e.g. in myocardial infarction
If a patient remains comatose following ROSC, then prognostication should be delayed for 72 hours to allow for neurological recovery.
Making decisions about CPR
There are several decisions regarding CPR that may need to be made. The most obvious is when to stop CPR, but there are also those that should take place before a patient goes into cardiac arrest.
Care planning and DNACPR
CPR is an invasive process and has a low success rate, as well as carrying risks, such as rib fractures, and long-term adverse outcomes from prolonged resuscitation attempts, such as hypoxic brain injury. Because of this, CPR is not appropriate for every patient who has a cardiac arrest.
A do not attempt cardiopulmonary resuscitation order (DNACPR) is a document (commonly completed as part of a ReSPECT form now) that formalises the decision about whether CPR would be started in the case of cardiac arrest. This decision may be made in cases where it is thought that CPR would be futile, that the risks of CPR outweigh any potential benefits or in line with a patient’s wishes.
DNACPR discussions often occur as patients reach the final stages of life. However, they should ideally be undertaken in advance of a patient’s deterioration to enable informed discussions with the patient and their family or carers.
An important exception to a DNACPR is a cardiac arrest caused by an unanticipated and easily reversible cause, such as choking or anaphylaxis. In these situations, it may be appropriate for resuscitation to be started. For example, if a patient with metastatic cancer has a DNACPR but has a cardiac arrest due to anaphylaxis from chemotherapy, then full resuscitation measures may be appropriate.
Conversations with patients and their families are never easy, but the Geeky Medics articles on advance care planning and DNACPR discussions contain more information and guidance.
Deciding to stop CPR
When deciding to stop ongoing CPR, several factors should be considered, including the patient’s background, response to any resuscitation measures tried so far, and the duration of the resuscitation attempt.
ALS guidelines state that CPR should generally be continued as long as there is a shockable rhythm or a potentially reversible cause of cardiac arrest that has not yet been treated. In cases of asystole, it is generally accepted that a duration of greater than 20 minutes, with no reversible cause and all ALS measures applied, is unlikely to be corrected with further CPR.
Ultimately, the decision to stop CPR in a hospital environment should be made by the team leader after discussion with others present if they feel that further ALS will not be successful.
In some situations, such as hypothermia, there is a greater chance of recovery without neurological damage, even in extended periods of cardiac arrest. In these cases, CPR should continue until warming has been achieved (i.e. the reversible problem is corrected).
Paramedics have specific criteria for when they may cease resuscitation during a pre-hospital cardiac arrest. The Geeky Medics guide to pre-hospital ALS provides further information.
Reviewer
Dr Sandeep Jutla
Emergency Medicine Consultant
Editor
Dr Jamie Scriven
References
- Resuscitation Council UK. Adult advanced life support Guidelines. 2021. Available from: [LINK]
- Resuscitation Council UK. Post-resuscitation care Guidelines. 2012. Available from: [LINK]
- Resuscitation Council UK. Special Circumstances Guidelines. 2021. Available from: [LINK]
- National Water Safety Forum. A future without drowning: The UK Drowning Prevention Strategy 2016-2026. 2015. Available from: [LINK]
- The Sepsis Trust. Yellow Manual – 6th Edition. 2022. Available from: [LINK]
- The British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. Decisions relating to cardiopulmonary resuscitation. 2016. Available from: [LINK]
Image references
- Figure 1. Adult advanced life support. 2021. Reproduced with the kind permission of Resuscitation Council UK.
- Figure 2. Adult tachycardia. 2021. Reproduced with the kind permission of Resuscitation Council UK.
- Figure 3. Adult bradycardia. 2021. Reproduced with the kind permission of Resuscitation Council UK.
Discover more from Bibliobazar Digi Books
Subscribe to get the latest posts sent to your email.




